Orthopedic Specialist Bruce Steinberg Explains Symptoms and Surgical Techniques for Treating Thumb Arthritis
By Dr. Bruce Steinberg
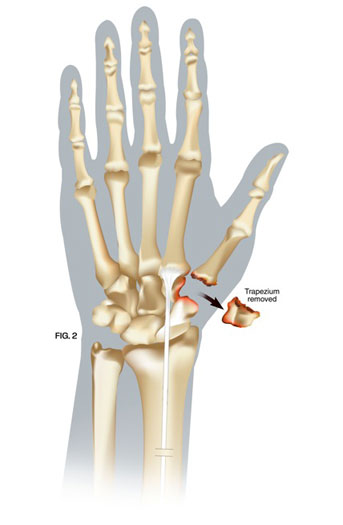
One of the most common causes of pain when pinching, grasping, torquing (twisting), and lifting with the hand, is arthritis at the base of the thumb. A complex saddle-shaped joint at the base of the thumb allows for movement of the thumb away from the palm. This joint also allows the thumb to pivot and turn so as to meet one or all of the fingers in opposition, which one might visualize as the thumb touching each of the fingertips. This complex function requires that the thumb be strong, flexible, and stable. The forces generated at the thumb base joint are extremely high. In a simple pinching maneuver, the force is 12 times greater at the base of the thumb than it is at the tip of the thumb. A lifetime of use, or trauma, may lead to osteoarthritis of this joint, the trapeziometacarpal joint, which is located between the trapezium and first metacarpal (see figure 1). Even the simplest tasks of daily living such as turning a key, grasping a doorknob, opening a car door, buttoning a shirt, or brushing ones’ teeth, can become impossible when one suffers from trapeziometacarpal joint arthritis. Osteoarthritis of this joint is most commonly seen in middle-aged or postmenopausal women. Female prevalence of this degenerative process is most likely due to greater joint laxity which leads to increased joint incongruity (the two sides of the joint don’t line up smoothly and evenly). Combining joint incongruity with high frequent forces leads to an accelerated degenerative process (osteoarthritis).
A careful clinical examination of the thumb and x-rays will make the diagnosis of osteoarthritis of the trapeziometacarpal joint. There are many treatments for trapeziometacarpal joint arthritis. Rest and non-steroidal anti-inflammatory medications should be the first step. If this fails, the treating physician may wish to try a Medrol Dosepak and consider a custom designed splint for the hand and thumb. An occupational therapist with special splint training is best equipped to make a hand based splint that incorporates the thumb. Unfortunately, most patients have difficulty tolerating the splint since it reduces thumb function considerably by limiting mobility of the trapeziometacarpal joint. Another option is an injection of corticosteroid into the trapeziometacarpal joint. The injection will usually resolve the pain in the early stages of arthritis; advanced stages may have no improvement. If there is no improvement in pain despite the previously described conservative efforts, the next step would be to consider surgical intervention.
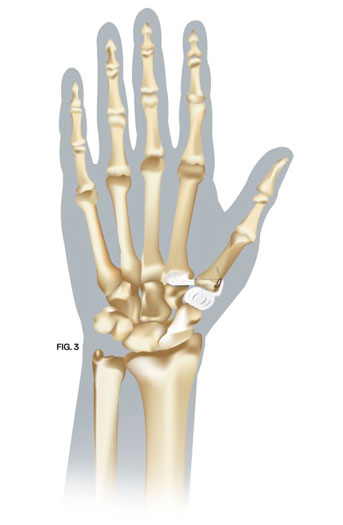
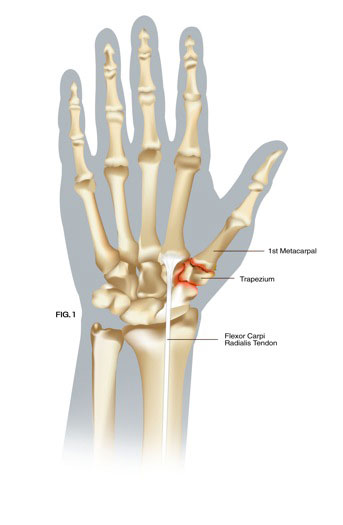
A surgical technique has been developed that is designed to last a lifetime. In this surgery, the arthritis at the base of the thumb is removed (see figure 2). An extra wrist flexor tendon, the flexor carpi radialis tendon, is released in the mid-forearm and placed through the bone at the base of the thumb (see figure 3). It is secured under tension to the base of the thumb by using a suture arising from an anchor. This tendon is then channeled underneath the base of the thumb and weaved back and forth to itself to fill the space created by the removal of the arthritic bone. Because the blood supply to the tendon has not been disrupted, this living joint replacement tissue becomes stronger with time. This surgical procedure takes less than an hour to complete in an outpatient setting. Therapy is started after 10 days and the protective splint is worn for 6 weeks following surgery. Long-term follow up studies have shown 95% of patients experiencing excellent relief of pain while also restoring thumb function.